Operative Hysteroscopy: A Comprehensive Guide to Modern Gynecological Surgery

Operative hysteroscopy stands as a groundbreaking advancement in gynecological surgery, transforming how women’s reproductive health issues are diagnosed and treated. As a less invasive, highly precise procedure, it offers numerous benefits for both patients and healthcare providers, ensuring better outcomes, fewer complications, and faster recovery times. This in-depth overview explores the core aspects of operative hysteroscopy, its indications, technical nuances, benefits, and why it is becoming the preferred choice in modern gynecology.
Understanding Operative Hysteroscopy: What Is It?
Operative hysteroscopy is a minimally invasive surgical procedure performed within the uterine cavity using a specialized instrument called a hysteroscope. Unlike diagnostic hysteroscopy, which primarily visualizes the uterine cavity, operative hysteroscopy involves the use of surgical tools to treat various intrauterine conditions without the need for abdominal incisions.
This technique leverages sophisticated optics and precise instrumentation to access the uterus through the cervix, significantly reducing patient discomfort, anesthesia requirements, and recovery time. The procedure is typically performed on an outpatient basis, enabling women to resume normal activities swiftly after treatment.
Technical Aspects and Procedure of Operative Hysteroscopy
Preparation and Patient Evaluation
Before proceeding with operative hysteroscopy, comprehensive patient evaluation is essential. This includes detailed medical history, pelvic examination, and imaging studies such as ultrasound or MRI. Laboratory tests, including blood counts and coagulation profiles, are also conducted to ensure patient safety.
Procedure Steps
- Patient positioning: Typically in a lithotomy position to provide optimal access to the cervix.
- Anesthesia: Local, regional, or general anesthesia is chosen based on the extent of the procedure and patient preference.
- Cervical dilation: The cervix is gently dilated if necessary to facilitate hysteroscope insertion.
- Insertion of hysteroscope: A thin, tubular instrument equipped with a camera and light is carefully inserted through the cervix into the uterine cavity.
- Visualization and assessment: The uterine cavity is examined in detail for pathology such as fibroids, polyps, septa, adhesions, or congenital anomalies.
- Therapeutic intervention: Using specialized instruments passed through the hysteroscope, the surgeon performs procedures like polypectomy, myomectomy, septum resection, or adhesiolysis.
- Completion and withdrawal: After the successful treatment, the hysteroscope is gently removed, often with minimal discomfort.
Indications for Operative Hysteroscopy
The versatility of operative hysteroscopy makes it applicable for a wide range of gynecological conditions. It is recommended in the following scenarios:
- Intrauterine polyps: For removal of benign growths causing abnormal bleeding or infertility.
- Submucous fibroids: To excise fibroids that distort the uterine cavity and impair fertility.
- Congenital uterine anomalies: Such as septa or duplications, which can affect pregnancy outcomes.
- Asherman's syndrome (intrauterine adhesions): To restore the uterine cavity and improve reproductive potential.
- Recurrent pregnancy loss: Diagnosing and treating intrauterine pathology that may contribute to early miscarriages.
- Heavy menstrual bleeding: When structural causes like polyps or fibroids are identified.
- Endometrial ablation: For treating abnormal uterine bleeding refractory to medical therapy.
Advantages of Operative Hysteroscopy
Compared to traditional open or laparoscopic surgeries, operative hysteroscopy offers numerous advantages that make it the preferred modality for suitable candidates:
- Minimally invasive: No external incisions are required, reducing pain and scarring.
- High precision: Direct visualization allows targeted treatment of intrauterine pathology.
- Reduced risk of complications: Less bleeding, infection, and damage to surrounding tissues.
- Shorter hospital stays: Often performed as an outpatient procedure with same-day discharge.
- Faster recovery: Women typically resume normal activities within a day or two.
- Enhanced diagnostic accuracy: Real-time imaging facilitates precise diagnosis and immediate therapeutic intervention.
- Cost-effective: Less resource-intensive and associated with lower healthcare costs.
- Increased patient comfort: Reduced anesthesia requirements and minimal postoperative discomfort.
Technological Innovations in Operative Hysteroscopy
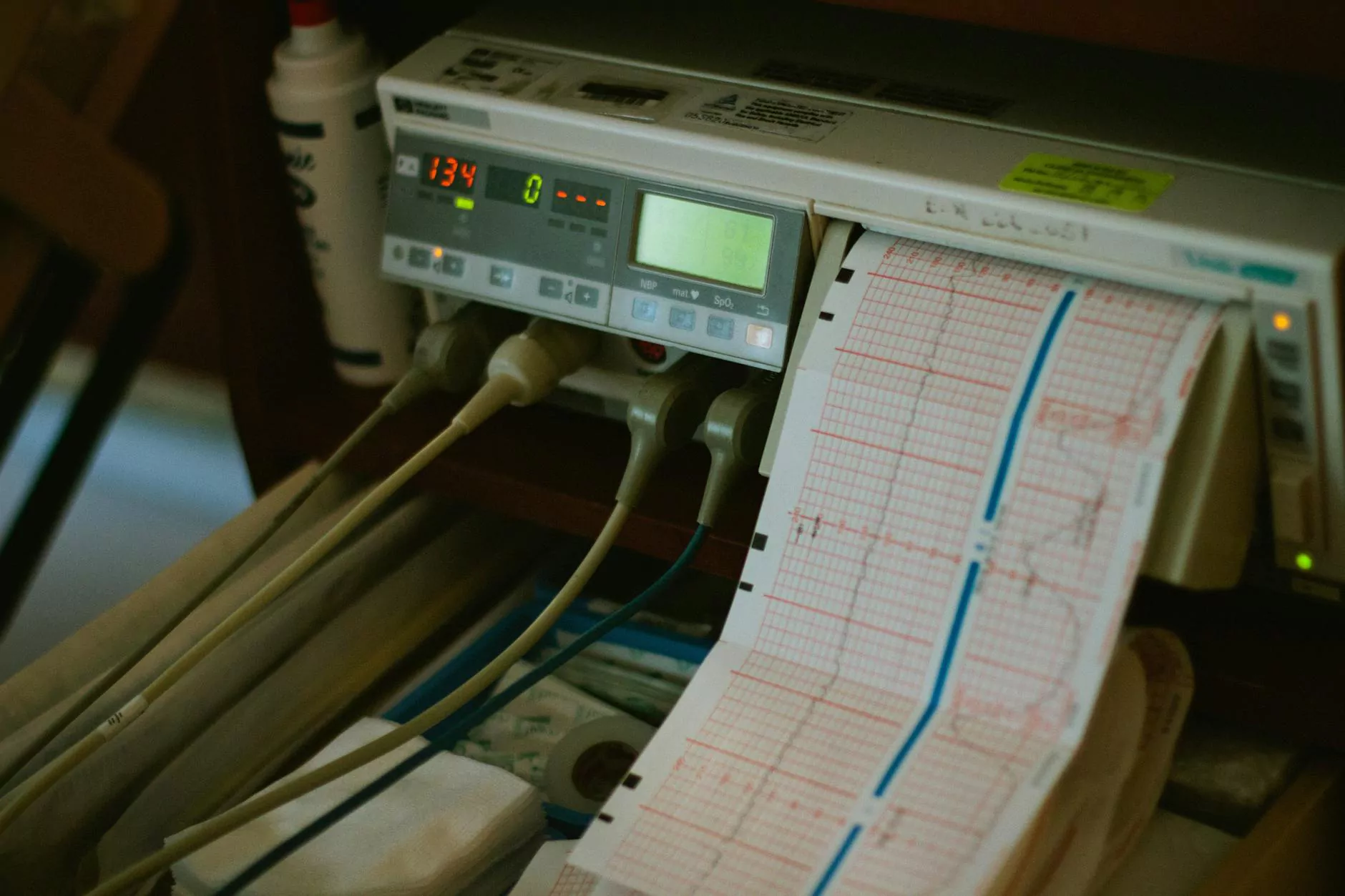
Advances in hysteroscopic technology continue to expand its capabilities and safety profile:
- High-definition cameras: Provide superior visualization of intrauterine structures.
- Fluid management systems: Ensure safe distension and minimize the risk of fluid overload.
- Miniaturized instruments: Allow for delicate manipulations and treatment of small lesions.
- Electrosurgical devices: Facilitate precise cutting, coagulation, and tissue removal.
- Hybrid techniques: Combining hysteroscopy with ultrasound or other imaging modalities for enhanced accuracy.
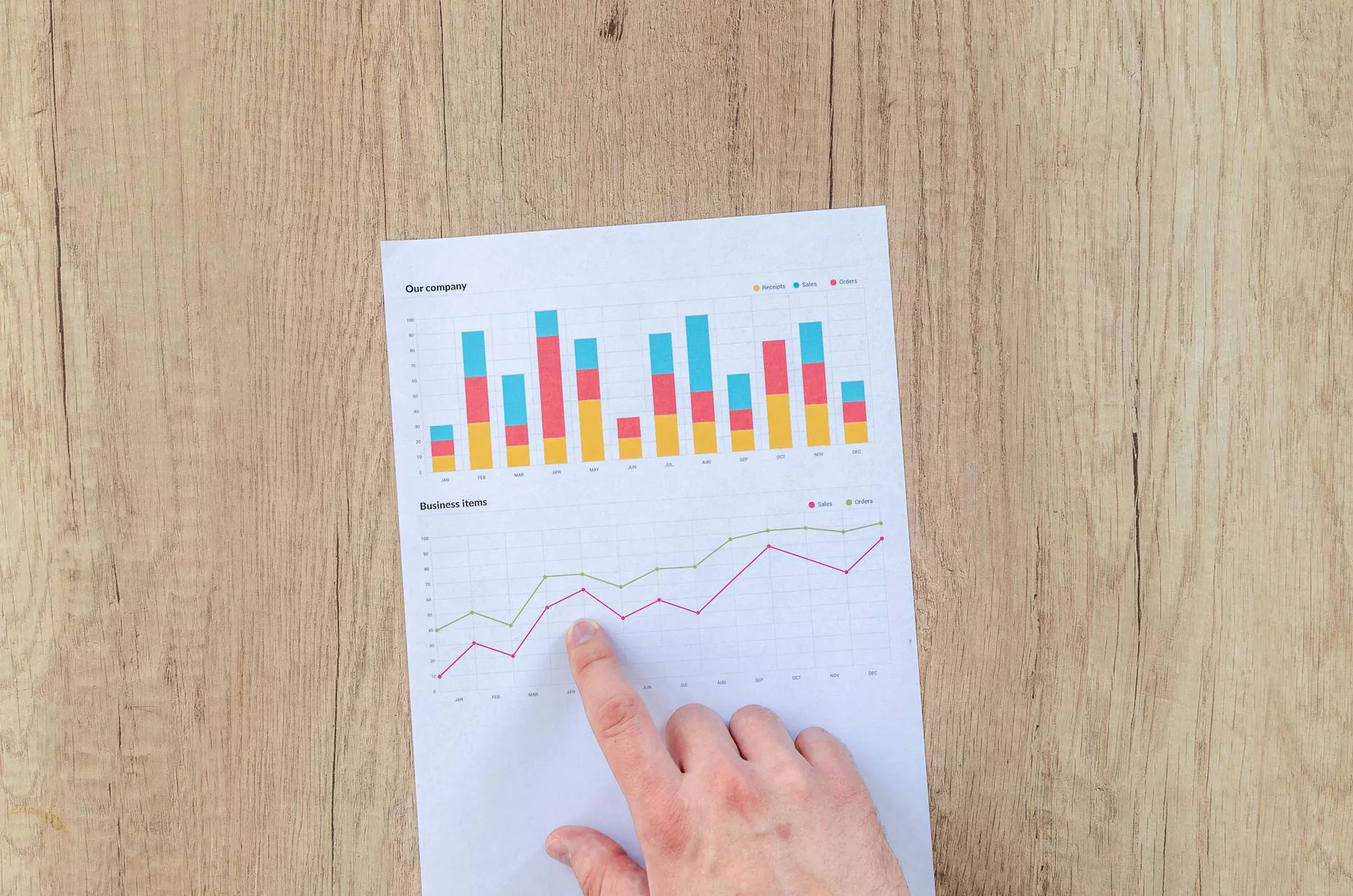
Clinical Outcomes and Success Rates
Operative hysteroscopy has demonstrated excellent clinical outcomes across multiple studies and clinical practices worldwide. Success rates depend on the specific condition being treated but generally include:
- High rate of symptom resolution: Such as bleeding, infertility, or recurrent miscarriage.
- Restoration of normal uterine anatomy: Especially in cases of adhesions or septa.
- Improved fertility outcomes: Many women experience increased chances of conception post-procedure.
- Low complication rates: Less than 1-2% in experienced hands.
Choosing the Right Specialist for Operative Hysteroscopy
Given the precision and technical expertise required, selecting a skilled and experienced obstetrician or gynecologist specializing in minimally invasive gynecological procedures is crucial. At drseckin.com, leading specialists incorporate the latest techniques and technologies to ensure optimal outcomes. Their expertise in operative hysteroscopy guarantees that each patient receives personalized, comprehensive care tailored to her unique gynecological needs.
The Future of Operative Hysteroscopy in Gynecology
The field of gynecological surgery is rapidly evolving, with operative hysteroscopy at the forefront. Future developments include the integration of robotic systems, improved visualization tools, and enhanced tissue management devices. These innovations will further refine the procedure's safety, efficacy, and scope, making it accessible to even wider patient populations.
Conclusion: Embracing a New Era in Women’s Reproductive Health
In conclusion, operative hysteroscopy embodies the essence of modern minimally invasive gynecological treatment. Its ability to accurately diagnose and effectively treat intrauterine pathology with minimal discomfort and downtime makes it a cornerstone of contemporary reproductive health care. As technology advances and surgical expertise deepens, women benefit from safer procedures, improved reproductive outcomes, and enhanced quality of life.
For women seeking expert evaluation and treatment using operative hysteroscopy, trust the experienced team at drseckin.com—your premier destination for innovative gynecological care.